
How to Cure Arthritis in Feet: A Step-by-Step Guide
Foot pain is never just about your feet. It’s about the morning stiffness that makes getting out of bed a challenge, the walks you have to cut short, and the activities you start to avoid. When foot arthritis is the cause, it can feel like it’s slowly chipping away at your freedom and mobility. The real question isn’t just how to cure arthritis in feet, but how to build a life where pain doesn’t dictate your daily choices. The most effective treatment plans look at the whole picture. This guide will explore a comprehensive approach, covering everything from anti-inflammatory diet tips and supportive footwear to advanced, non-invasive therapies that help reduce pain and inflammation without side effects, empowering you to manage your condition holistically.
Key Takeaways
- Your Daily Choices Have the Biggest Impact: Small, consistent actions like choosing supportive shoes, staying active with low-impact exercise, and managing your weight are the foundation for controlling arthritis symptoms and protecting your joints.
- Combine Treatments for Better Results: The most effective pain management strategy layers different approaches. Pair your at-home care with professional options like physical therapy or non-invasive light therapy to address discomfort from every angle.
- A Proper Diagnosis is Your Starting Point: Don't let myths or guesswork dictate your care. Understanding the true cause of your foot pain is the critical first step to building a personalized treatment plan that brings real relief.
What Is Foot Arthritis?
If you’ve ever felt a persistent ache, pain, or stiffness in your feet, you might be dealing with foot arthritis. Simply put, it’s inflammation in any of the more than 30 joints in your feet and ankles. This inflammation can make simple movements like walking or standing feel like a major challenge. Understanding what’s happening inside your feet is the first step toward finding effective relief and getting back to the activities you love.
The Different Types of Arthritis in Feet
"Arthritis" is an umbrella term, and several types can affect your feet. The most common ones include:
- Osteoarthritis: Often called "wear-and-tear" arthritis, this happens when the protective cartilage that cushions your joints gradually wears down. As it disappears, bone can rub against bone, causing pain and stiffness.
- Rheumatoid Arthritis (RA): This is an autoimmune disease where your body’s immune system mistakenly attacks the lining of your joints. This can lead to painful swelling, redness, and can even weaken the bones over time.
- Gout: This type is caused by a buildup of uric acid crystals in a joint. It often strikes suddenly and intensely, frequently targeting the big toe.
Each type requires a different approach to pain management, so getting a clear diagnosis is key.
Key Symptoms to Watch For
Foot arthritis symptoms can range from mild to severe and may come and go. Being aware of the early signs can help you address the issue before it gets worse. Keep an eye out for these common symptoms:
- Pain in the joints, especially during or after movement.
- Stiffness that makes it difficult to move your foot, ankle, or toes, particularly in the morning or after sitting for a while.
- Swelling in or around the joint area.
- A reduced range of motion, meaning you can’t move your foot or ankle as freely as you used to.
- Changes in the skin around the joint, such as redness or warmth to the touch.
If these symptoms sound familiar, it’s a good idea to talk to a healthcare professional.
Common Causes of Foot Arthritis
So, what causes foot arthritis to develop? It’s often a combination of factors rather than a single trigger. Some of the most common causes and risk factors include:
- Age and general wear: The cartilage in our joints can naturally wear down over a lifetime of use.
- Previous injuries: A past sprain, fracture, or other injury to your foot or ankle can increase your risk of developing arthritis in that joint later on.
- Family history: If your parents or siblings have arthritis, you may be more likely to develop it, too.
- Other health conditions: Issues like obesity, which puts extra stress on your foot joints, and autoimmune diseases can contribute to arthritis.
Focusing on preventative wellness by maintaining a healthy weight and protecting your feet from injury can make a big difference.
Lifestyle Changes to Help Manage Foot Arthritis
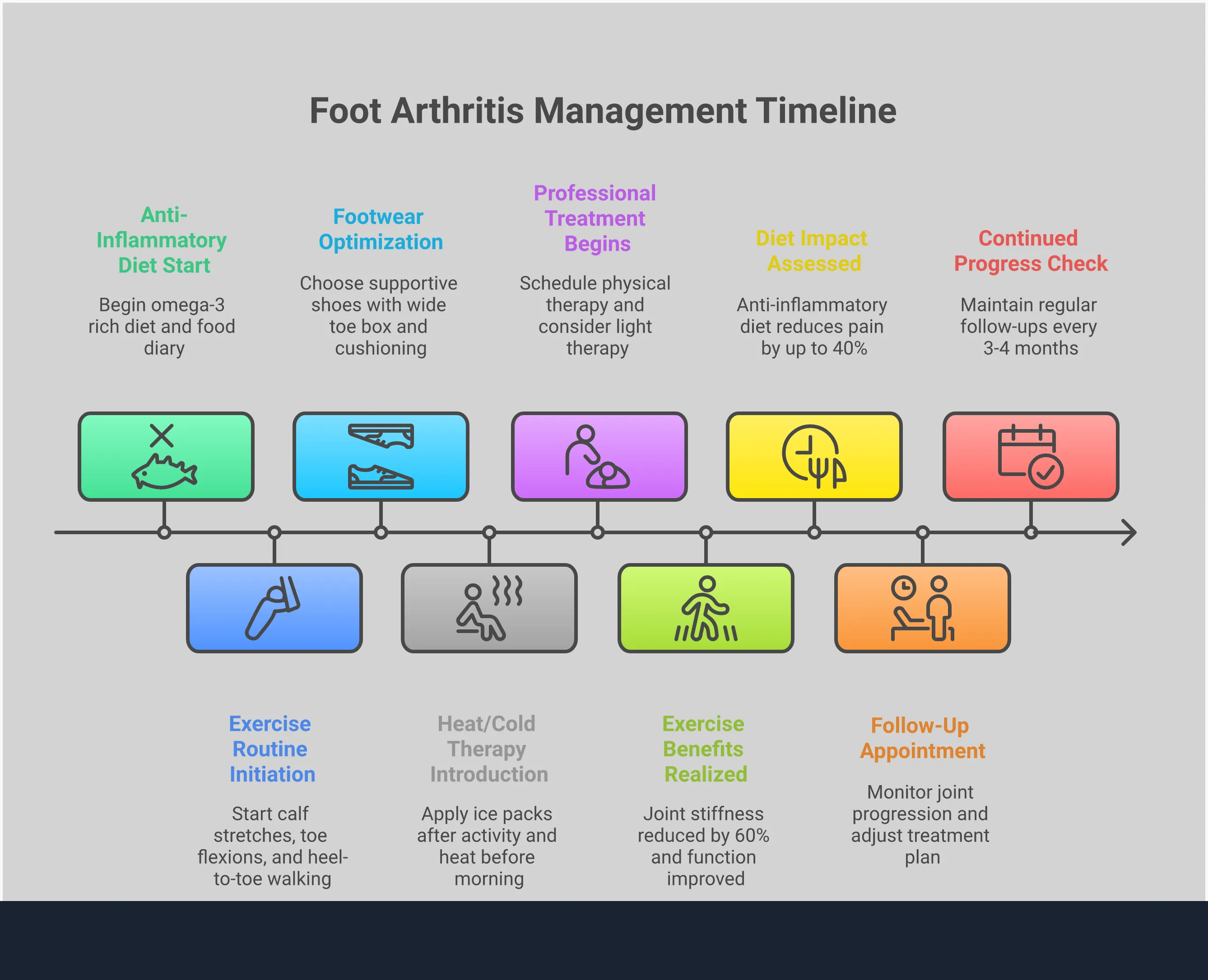
While professional treatments are a cornerstone of managing foot arthritis, the small choices you make every day have a significant impact on your pain levels and mobility. Integrating a few key lifestyle adjustments can help you feel more in control of your symptoms and support your overall treatment plan. These changes focus on reducing stress on your joints, improving flexibility, and providing immediate relief when you need it most.
Fine-Tune Your Diet and Weight
Your feet carry your entire body, so managing your weight is one of the most effective ways to ease the pressure on those sensitive joints. Research shows that losing even a small amount of weight can significantly reduce stress on your foot joints, which can lead to less pain and inflammation. Think of it as lightening the load your feet have to bear with every step. Alongside weight management, focusing on an anti-inflammatory diet rich in fruits, vegetables, lean proteins, and healthy fats can also help manage arthritis symptoms from the inside out. Small, consistent changes to your diet can make a world of difference in how your feet feel day-to-day.
Embrace Low-Impact Exercise and Stretching
When your feet hurt, the last thing you might want to do is move. However, the right kind of movement is crucial for keeping your joints from getting stiffer. Low-impact exercises like swimming, cycling, and walking are fantastic for staying active without jarring your joints. They help maintain mobility and can even reduce pain over time. Gentle stretching is also your best friend for stiff, swollen feet. Try a simple calf stretch against a wall or use an exercise band to gently pull your toes back. These simple movements improve flexibility and can provide immediate relief, making it easier to get through your day with less discomfort.
Choose the Right Footwear
The shoes you wear can either be a source of relief or a major cause of pain. The right pair acts as a support system for your feet. When shopping for shoes, look for a few key features: a wide toe box that gives your toes plenty of room, a firm sole that doesn't bend too easily in the middle, and good arch support. Shoes that match the natural shape of your foot and have flexible, rubber soles will provide the best combination of comfort and stability. Investing in proper footwear is a simple but powerful step toward better pain management and improved mobility.
Use Heat and Cold Therapy
Heat and cold therapy are simple, effective, and accessible tools for managing daily arthritis symptoms. The general rule is easy to remember: use ice for inflammation and heat for stiffness. If your feet are swollen and achy after a long day, applying an ice pack (wrapped in a towel) for about 20 minutes can help reduce the inflammation. If you wake up with stiff, sore joints, a heating pad or a warm foot soak can help relax the muscles and improve blood flow before you start your day. Alternating between the two can be a great way to address both pain and stiffness as they arise.
Medical Treatments for Foot Arthritis
When lifestyle adjustments aren't quite cutting it, several medical treatments can step in to provide more significant relief from foot arthritis. Working with your doctor is the best way to figure out which path is right for you. They can properly diagnose your condition using a physical exam, X-rays, or other tests to see what’s happening inside your joints. From there, you can explore options that range from medication to innovative, non-invasive therapies designed to reduce pain and improve your mobility. The goal is always to find a sustainable solution that helps you get back to doing what you love, with less discomfort holding you back.
Medication Options
Medications are often one of the first lines of defense for managing arthritis pain and swelling. Your doctor might start by recommending over-the-counter pain relievers like ibuprofen or acetaminophen to see if they provide enough relief for your day-to-day activities. If your symptoms are more persistent, they may suggest prescription-strength anti-inflammatory drugs. For more intense flare-ups, corticosteroid shots administered directly into the affected joint can offer powerful, short-term relief. While these options can be effective for managing symptoms, they don’t address the underlying joint damage and are best used as part of a broader treatment plan.
Physical Therapy
Physical therapy is a fantastic, hands-on approach to managing foot arthritis. A skilled physical therapist can design a program specifically for you, focusing on exercises that strengthen the muscles supporting your foot and ankle joints. This added support helps reduce stress on the joints themselves. Gentle stretching routines can also improve your flexibility and range of motion, making it easier to walk and stay active. Your therapist can also guide you on proper movement patterns to avoid putting unnecessary strain on your feet. It’s an empowering process that gives you the tools to actively participate in your own recovery and long-term joint health.
Injections and Custom Orthotics
For more targeted relief, your doctor might recommend a combination of treatments. Corticosteroid injections, for example, can deliver strong anti-inflammatory medicine directly to the source of your pain, helping to calm a severe flare-up. While injections provide temporary relief, custom shoe inserts, or orthotics, offer a long-term support solution. Unlike the inserts you buy at the store, custom orthotics are molded to your feet to correct alignment issues, cushion sensitive areas, and distribute pressure more evenly as you walk. This can significantly lessen pain and help prevent further joint damage by providing stability where you need it most.
Light Therapy for Natural Relief
If you’re looking for a drug-free, non-invasive way to manage foot arthritis, light therapy is an excellent option. This advanced treatment uses specific wavelengths of light to penetrate deep into your tissues, where it helps reduce inflammation and stimulate your body's natural healing processes at a cellular level. It’s a gentle and painless way to find lasting relief from chronic pain without the side effects of medication or the recovery time of surgery. At Laser Lab, we use light therapy to help our clients get back on their feet and enjoy life with less pain. Our approach to pain management is focused on helping your body heal itself from the inside out.
When Is Surgery the Right Option?
Deciding to have surgery is a major step, and it’s usually considered only after you’ve explored every other avenue. For many people, a combination of lifestyle adjustments, physical therapy, and non-invasive treatments provides significant relief from foot arthritis. At Laser Lab Therapy, we’ve seen firsthand how powerful natural, light-based care can be for managing chronic pain and improving mobility without drugs or downtime.
However, there are times when the damage to a joint is so severe that these conservative treatments no longer provide the relief you need to live your life comfortably. If you’re experiencing constant pain that keeps you from walking, working, or doing the things you love, it might be time to have a conversation with your doctor about surgical options. Surgery is a last resort, but for the right person, it can be a path toward restoring function and finding long-term relief when nothing else has worked. The goal is always to get you back on your feet, and sometimes, surgery is the most direct route to get there.
Signs Your Current Treatments Aren't Enough
So, how do you know when you’ve reached that point? The clearest sign is persistent, severe pain that doesn’t respond to medication, physical therapy, or other interventions. If your mobility is severely limited and your quality of life is suffering, it’s time to talk to a specialist.
Your doctor will perform a physical exam, ask detailed questions about your symptoms, and may watch you walk to assess your gait. To get a clear picture of what’s happening inside your foot, they will likely order imaging tests. According to the Cleveland Clinic, these can include X-rays to see bone damage, or an MRI or CT scan to get a better look at the soft tissues and cartilage.
An Overview of Foot Arthritis Surgeries
If your doctor determines that surgery is the best course of action, there are a few different procedures they might recommend. The choice depends on which joint is affected and the extent of the damage.
According to NYU Langone Health, common surgical options include arthroscopic debridement, where the surgeon cleans out inflamed tissue and bone spurs from the joint. Another option is arthrodesis, or joint fusion, which involves fusing the bones together to eliminate painful movement. For severe cases, your doctor might suggest a joint replacement, where the damaged joint is replaced with an artificial one. Each of these procedures is a significant undertaking, which is why they are reserved for when other treatments fail.
What to Expect During Recovery
Recovery from foot surgery requires patience and a commitment to following your doctor’s instructions. It’s not a quick fix, and you’ll need to plan for a period of downtime.
After most foot arthritis surgeries, you can expect to be off your feet for a while. According to experts at the Hospital for Special Surgery, you may need to avoid putting any weight on your foot for two to six weeks. You’ll also need to coordinate with your medical team to manage any medications you’re taking, as some can interfere with the healing process. Physical therapy will be a key part of your recovery, helping you gradually regain strength, flexibility, and range of motion in your foot and ankle.
Understanding the Risks
Like any major medical procedure, foot surgery comes with potential risks. It’s important to go into it with a clear understanding of the possible complications so you can make an informed decision with your healthcare provider.
Potential risks include infection at the incision site, blood clots, nerve damage, and adverse reactions to anesthesia. There’s also a chance the surgery may not fully relieve your pain or that the arthritis could develop in adjacent joints over time. These risks are why surgeons are often cautious and recommend exhausting all non-invasive options first. Exploring treatments that support your body’s natural healing ability can help you manage symptoms effectively and may delay or even prevent the need for surgery.
Building Your Personalized Treatment Plan
Finding relief from foot arthritis is less about a single magic bullet and more about creating a smart, sustainable strategy that fits your life. The most effective approach is a personalized one that combines daily habits with professional guidance. The goal is to lessen your pain, protect your joints from further damage, and get you back to doing the things you love. By taking an active role in your care, you can build a plan that truly works for you, addressing your specific symptoms and health goals.
Combining At-Home Care and Professional Treatments
The best way to manage foot arthritis is by pairing consistent at-home care with effective professional treatments. Think of it as a partnership. At home, you can focus on things like gentle stretching, using hot or cold packs to soothe discomfort, and choosing supportive footwear. These daily actions lay the foundation for long-term comfort. When you combine these habits with professional care, you amplify your results. Treatments like light therapy offer a powerful, non-invasive way to target inflammation and pain at the source, providing relief that at-home methods alone might not achieve. This integrated approach ensures you’re tackling the problem from every angle for more comprehensive pain management.
Partnering With Your Healthcare Team
You don’t have to figure this all out on your own. Assembling a trusted healthcare team is one of the most important steps you can take. This team might include your primary doctor, a podiatrist, a physical therapist, and a specialist like a rheumatologist if needed. Each professional brings a different perspective to help create a well-rounded plan. Be open with them about your symptoms, your lifestyle, and what you hope to achieve. At Laser Lab Therapy, we see ourselves as a key part of your wellness team, working with you to provide natural, drug-free relief that complements your overall health strategy. Finding practitioners you can trust and communicate with makes all the difference.
Setting Realistic Goals for Your Health
Managing arthritis is a marathon, not a sprint. Setting realistic, achievable goals is key to staying motivated and seeing real progress. Instead of aiming for a complete "cure," focus on tangible improvements. Maybe your goal is to walk around the block without pain, reduce your reliance on pain medication, or simply have more energy for your family. Your ideal treatment plan will be unique to your body and your goals. It involves finding the right mix of exercise, stress management, and treatments that work for you. By focusing on preventative wellness and consistent daily habits, you can create a new normal where arthritis doesn't call the shots.
How to Keep Foot Arthritis from Progressing
Receiving an arthritis diagnosis can feel like a roadblock, but it’s really a call to be more intentional with your foot health. By taking proactive steps, you can manage your symptoms and slow the progression of the condition. It’s about shifting your focus from simply reacting to pain to building a lifestyle that supports your joints for the long run. These strategies aren’t about a quick fix; they’re about creating a sustainable routine that keeps you moving comfortably and confidently. Think of it as taking control of your health, one step at a time.
Daily Habits to Protect Your Feet
Small, consistent changes in your daily routine can make a world of difference for your feet. If you're carrying extra weight, even a small loss can significantly lighten the load on your joints. Think of your shoes as your feet's support system—look for pairs with a wide toe box that gives your toes room to breathe, a firm sole, and solid arch support. Staying active is also crucial, but you want to be kind to your joints. Low-impact activities like swimming, cycling, or walking are fantastic for maintaining mobility without putting your feet through unnecessary stress.
Important Warning Signs
It’s easy to brush off aches and pains as a normal part of life, but your body often sends clear signals when it needs attention. A persistent ache in your feet or ankles isn't something you just have to live with. It’s time to check in with a healthcare provider if you experience severe pain that lasts more than a week, stiffness that seems to be getting worse, or frequent flare-ups of your arthritis symptoms. Listening to these warning signs and seeking advice early can help you get the right care before the condition worsens.
Strategies for Long-Term Foot Health
While there isn't a magic cure for arthritis, you have many tools at your disposal to manage it effectively and live comfortably. Consistent, moderate movement is one of the best things you can do for your joints, helping to reduce stiffness and maintain function. A great long-term plan often combines several approaches, from custom shoe inserts to physical therapy. For those seeking a drug-free way to handle inflammation and discomfort, non-invasive options can be a cornerstone of your pain management strategy. The key is to find a combination of treatments that works for your body and lifestyle.
Foot Arthritis Myths vs. Facts
When you’re dealing with foot pain, it’s easy to get overwhelmed by conflicting advice. Misinformation about arthritis can keep you from finding real relief and may even make your symptoms worse. Let’s clear up some of the most common myths about foot arthritis so you can focus on what actually works. Understanding the facts is the first step toward creating a management plan that helps you feel and move better. By separating fiction from reality, you can take control of your foot health with confidence.
Is It Just an Age-Related Problem?
One of the biggest myths is that arthritis is something only older adults have to worry about. While it’s true that the risk increases with age, arthritis can affect anyone, at any stage of life. In fact, the Centers for Disease Control and Prevention (CDC) reports that nearly 300,000 children in the U.S. have some form of arthritis. Believing it’s just a part of getting older can cause people to delay seeking help. The truth is, getting an early diagnosis and starting a proactive pain management plan is key to managing symptoms and protecting your joints for the long haul, no matter how old you are.
The Truth About Activity and Rest
When your feet hurt, your first instinct might be to stay off them as much as possible. It seems logical that resting your joints would prevent further pain, but the opposite is often true. While you should avoid activities that cause sharp pain, complete inactivity can lead to stiffness and weaker muscles, making your arthritis symptoms worse. The fact is, moderate physical activity is one of the best things you can do for your joints. Low-impact exercises like swimming, cycling, and gentle stretching can reduce pain, improve flexibility, and strengthen the muscles that support your feet, leading to a better quality of life.
Misconceptions About Managing Pain
It’s easy to feel discouraged and believe there’s nothing you can do about arthritis pain. This is simply not true. While arthritis is a chronic condition, it is absolutely manageable. A combination of lifestyle adjustments, targeted exercises, and effective treatments can make a significant difference in your daily comfort and mobility. Another common mistake is assuming that all joint pain is arthritis. Conditions like tendonitis or bursitis can cause similar symptoms, which is why a proper diagnosis is so important. Working with a professional helps you understand the true cause of your pain and find a personalized care strategy that works for you.
Frequently Asked Questions
I think I have foot arthritis. What's the very first thing I should do? The most important first step is to get a proper diagnosis from a healthcare professional, like your doctor or a podiatrist. Self-diagnosing can lead you down the wrong path, as different types of joint pain require different approaches. A clear diagnosis is the foundation for creating a treatment plan that will actually bring you relief.
You mention exercise is good, but moving hurts. How do I start without making the pain worse? That’s a completely valid concern. The key is to choose movements that are kind to your joints. Start with low-impact activities like swimming, gentle cycling on a stationary bike, or simple seated stretches. The goal is to keep your joints mobile without jarring them. Always listen to your body; if you feel sharp pain, it’s a sign to ease up.
How does light therapy actually work for foot arthritis? Light therapy uses specific, safe wavelengths of light that penetrate through the skin to reach the inflamed tissues in your foot. This light helps calm inflammation at a cellular level and stimulates your body’s natural healing processes. It’s a gentle and effective way to address the pain and stiffness right at the source, without relying on medication.
Do I really need to buy expensive special shoes? Not always. While some people benefit from custom orthotics, you can often find relief by being a smart shopper. Look for shoes that have a wide toe box, good arch support, and a sole that is both firm and cushioned. The goal is support and stability, which you can find in many quality footwear brands without needing a special prescription.
Is it possible to live a normal, active life with foot arthritis? Yes, absolutely. Getting an arthritis diagnosis isn't a sentence to a sedentary life. It’s about learning how to manage the condition intelligently. By building a personalized plan that includes the right combination of daily habits, supportive care, and effective treatments, you can significantly reduce your symptoms and continue to live an active, fulfilling life.
Frequently Asked Questions
Is light therapy safe for athletes?

Yes, light therapy is completely safe and highly beneficial for athletes. It promotes faster muscle recovery, reduces inflammation, and supports performance without the risks of medication or downtime. That’s why professional and amateur athletes worldwide rely on it to train smarter and recover quicker.
How many sessions will I need?

The number of sessions varies depending on the type and severity of your condition. Many patients notice improvement after 3–5 sessions, while chronic conditions may require ongoing care for best results. During your initial consultation, we’ll design a personalized treatment schedule tailored to your body’s response and recovery goals.




