
What Causes Osteoarthritis? 5 Key Risk Factors
You’ve probably heard that osteoarthritis is just a normal part of getting older—a simple case of “wear and tear” on your joints. But this idea doesn’t tell the whole story and can leave you feeling like there’s nothing you can do. The truth about what causes osteoarthritis arthritis is far more complex and, surprisingly, more empowering. It involves a mix of your genetic predispositions, the impact of old injuries, and the effects of chronic inflammation. By moving past the myths, you can get a clearer picture of what’s really happening in your body and discover actionable strategies that address the root issues, not just the symptoms.
Key Takeaways
- You have more control than you think: Osteoarthritis isn't just inevitable "wear and tear." You can directly support your joint health by managing your weight, choosing anti-inflammatory foods, and being mindful of repetitive movements in your daily life.
- Movement is medicine for your joints: It might seem counterintuitive, but avoiding activity can make joint stiffness worse. Gentle exercises like walking or swimming strengthen the muscles around your joints, providing better support and easing discomfort.
- Address the root cause, not just the symptoms: Lasting relief comes from reducing the underlying inflammation that drives joint pain. Drug-free therapies like light therapy work at the cellular level to calm inflammation and support your body's healing process, offering a sustainable way to improve joint function.
What is Osteoarthritis?
If you've ever felt a deep, aching pain in your joints, especially after moving around, you might have wondered about arthritis. Osteoarthritis, or OA, is the most common type of arthritis, affecting millions of people. Think of it as the "wear and tear" kind. Inside your joints, you have a smooth, rubbery tissue called cartilage that acts as a cushion between your bones, allowing them to glide smoothly. Over time, this cartilage can start to break down and wear away. When that happens, the bones can begin to rub against each other, causing pain, stiffness, and swelling.
This process doesn't happen overnight. It's a gradual breakdown that often affects joints we use the most, like our knees, hips, hands, and spine. You might notice your joints feel stiff in the morning or that it's harder to do simple things like open a jar or walk up the stairs. While it’s true that the risk of developing OA increases with age, it's not just an "old person's disease." The good news is that understanding what's happening in your body is the first step toward finding effective pain management solutions. There are many ways to protect your joints and live comfortably, and you don't have to settle for a life limited by pain.
How Osteoarthritis Differs from Other Types of Arthritis
It's easy to hear "arthritis" and think it's all the same, but that's not the case. The key difference between osteoarthritis and other forms, like rheumatoid arthritis (RA), comes down to the cause. Osteoarthritis is a degenerative joint disease—it’s caused by mechanical wear and tear on your joints over many years.
Rheumatoid arthritis, on the other hand, is an autoimmune disorder. This means the body's own immune system gets confused and mistakenly attacks the lining of the joints, causing widespread inflammation. While both can cause joint pain, RA often affects joints symmetrically (both knees, for example) and can come with other symptoms like fatigue and fever. Understanding this distinction is crucial because it guides how you approach managing your symptoms and finding relief.
What Are the Primary Causes of Osteoarthritis?
When you’re dealing with stiff, aching joints, it’s natural to wonder where it all started. Osteoarthritis isn’t caused by a single event but is usually the result of several factors that affect your joints over time. Think of it as a combination of your body’s natural processes, your history, and your daily habits all coming together. Understanding these root causes is the first step toward finding effective, lasting pain management that goes beyond just masking the symptoms.
The primary driver behind osteoarthritis is the breakdown of cartilage, the firm, rubbery tissue that cushions the ends of your bones. But what causes that breakdown? It often comes down to three main areas: the natural wear of cartilage, the lasting impact of old injuries, and the cumulative effect of repetitive stress on your joints. By looking at each of these factors, you can get a clearer picture of what’s contributing to your discomfort and how to best support your joint health moving forward.
How Cartilage Breaks Down
Imagine the cartilage in your joints as the protective padding at the ends of your bones. Its job is to provide a smooth, gliding surface for motion and to act as a shock absorber. Osteoarthritis begins when this essential cushion starts to wear away. Over time, the cartilage can become thin, rough, and frayed. As it deteriorates, the space between the bones narrows, which can eventually lead to painful bone-on-bone contact. This process is often gradual, but it’s the central reason for the stiffness, swelling, and pain associated with osteoarthritis.
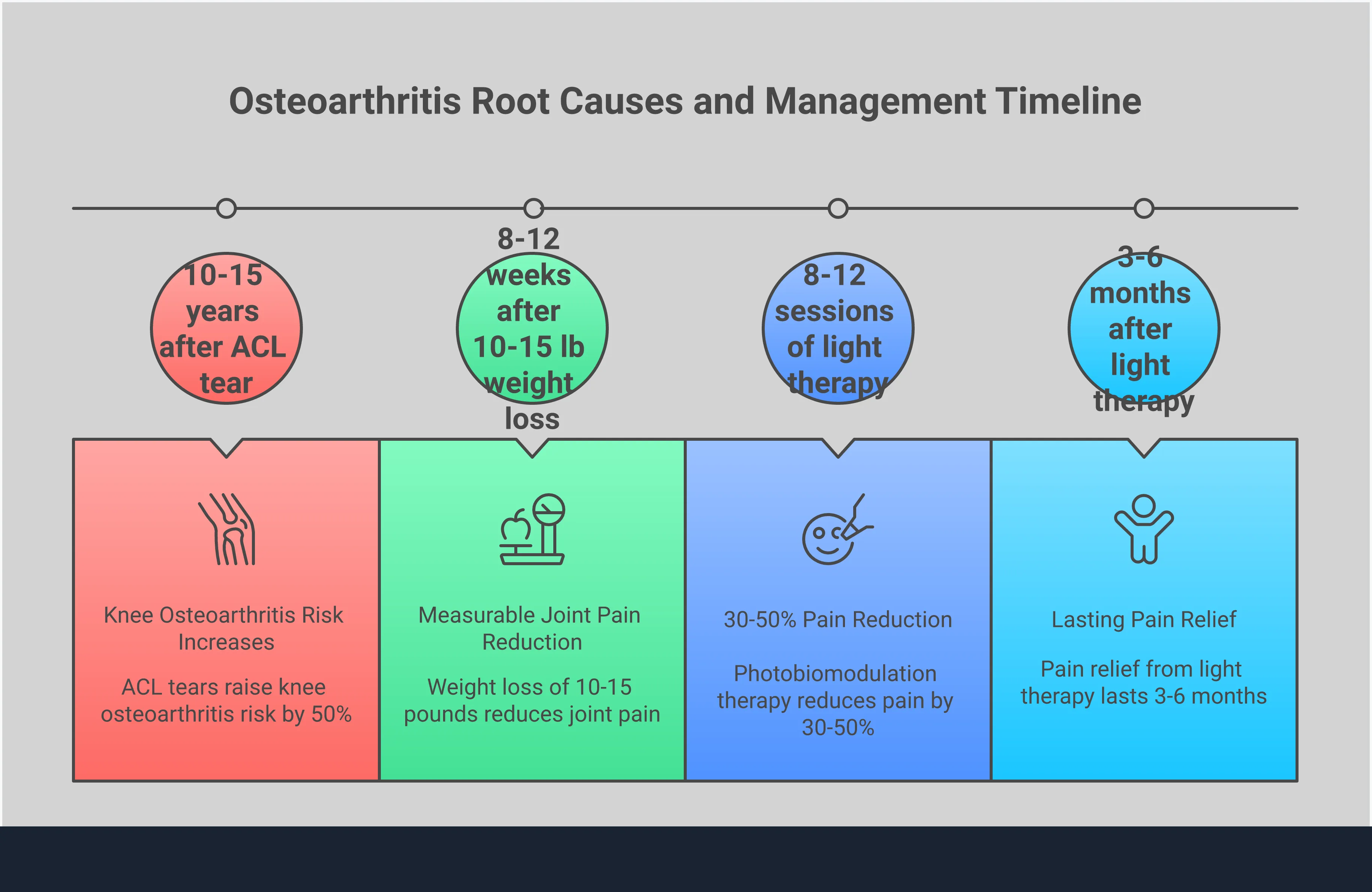
The Role of Joint Injuries and Trauma
A significant injury—whether from a car accident, a fall, or a sport—can set the stage for osteoarthritis years down the line, even if the injury seemed to heal completely. This is known as post-traumatic osteoarthritis. A fracture, ligament tear, or meniscus tear can alter the mechanics of your joint, placing uneven stress on the cartilage. This imbalance can speed up the wear-and-tear process. That’s why supporting your body’s natural healing process through proper performance recovery after an injury is so important for long-term joint health.
The Impact of Repetitive Stress
You don’t need a major injury to develop osteoarthritis. Sometimes, it’s the small, repeated movements over many years that contribute to cartilage breakdown. Jobs that require frequent kneeling, squatting, or heavy lifting can place consistent strain on the knees and hips. Even seemingly low-impact activities, like typing or playing a musical instrument, can lead to osteoarthritis in the hands if performed for hours every day. This repetitive stress gradually wears down the cartilage, highlighting how our daily routines and occupations can directly influence the health of our joints.
Are You at Risk for Osteoarthritis?
Understanding the factors that contribute to osteoarthritis is the first step in protecting your long-term joint health. While you can’t change your age or your genes, knowing your personal risk profile empowers you to make proactive choices. Several key factors can influence your likelihood of developing joint pain and stiffness, from your family history to your daily habits. Let's look at some of the most common risk factors.
Age and Joint Health
It’s true that the risk of developing osteoarthritis increases with age. Over the years, the protective cartilage that cushions our joints can gradually wear down. Think of it like the tread on a tire—with more miles, it naturally becomes thinner. This is why many people begin to notice symptoms of joint discomfort as they get older. However, this doesn’t mean joint pain is an inevitable part of aging. It simply means that being mindful of your joint health becomes even more important as you celebrate more birthdays.
How Extra Weight Affects Your Joints
Carrying even a few extra pounds can have a significant impact on your joints, especially the ones that bear your weight, like your knees and hips. This happens for two main reasons. First, the added weight places more additional stress on weight-bearing joints, which can speed up cartilage breakdown. Second, fat tissue isn't just passive weight; it produces proteins that can cause inflammation throughout your body, including in and around your joints. Managing your weight is one of the most effective ways to reduce your risk and ease existing symptoms.
Gender and Hormonal Factors
Studies show that women are more likely to develop osteoarthritis than men, particularly after the age of 50. Researchers believe this is linked to hormonal changes that occur during menopause. Estrogen is thought to have a protective effect on cartilage, so when estrogen levels decline, joints may become more vulnerable to damage and inflammation. This is an important factor for women to consider as part of their long-term wellness planning, focusing on joint-protective exercises and an anti-inflammatory diet.
Your Family History and Genetics
Have your parents or grandparents dealt with stiff, achy joints? If so, you might have a higher risk of developing osteoarthritis yourself. A family history of osteoarthritis suggests that certain genetic traits could be at play. These inherited factors might affect the composition of your cartilage, the way your joints are shaped, or your body's inflammatory response. While you can't change your genetic makeup, knowing your family history gives you a heads-up, encouraging you to adopt joint-friendly habits earlier in life to keep you moving comfortably for years to come.
How Your Lifestyle Affects Your Joints
While you can’t change your genetics or turn back the clock, you have a surprising amount of influence over your joint health through your daily habits. The choices you make every day—from what you eat to how you move—play a significant role in managing osteoarthritis symptoms and protecting your joints for the long haul. Focusing on these lifestyle factors is one of the most powerful ways to take control of your health and well-being.
The Connection Between Diet and Inflammation
What you eat can directly impact the level of inflammation in your body, which is a key driver of joint pain. Foods high in sugar, processed ingredients, and saturated fats can trigger or worsen inflammation, making your joints feel stiff and sore. On the other hand, filling your plate with anti-inflammatory foods can help calm things down. Think colorful fruits and vegetables, nuts, and fish rich in omega-3 fatty acids. Making small, consistent changes to your diet is a simple yet effective strategy for pain management and supporting your body from the inside out.
Your Activity Level and Exercise Habits
Movement is essential for healthy joints, but it’s all about finding the right balance. Regular, gentle exercise strengthens the muscles that support your joints, improves flexibility, and helps you maintain a healthy weight, which reduces stress on your knees and hips. Activities like walking, swimming, and cycling are fantastic options. However, it’s also important to listen to your body. Pushing too hard or using improper form can lead to injuries that accelerate joint damage. The goal is to stay active in a way that feels good and supports long-term joint function.
Workplace and Repetitive Motion Risks
Your job or even your hobbies could be putting extra strain on your joints. Occupations that involve repetitive motions—like typing, assembly line work, or heavy lifting—can cause gradual wear and tear on your cartilage over time. This doesn't mean you need to switch careers, but it does mean being mindful is key. You can protect your joints by taking regular breaks to stretch, using ergonomic tools and equipment, and focusing on proper posture. These small adjustments can make a big difference in reducing cumulative stress and preserving your joint health for years to come.
Common Myths About Osteoarthritis Causes
When it comes to osteoarthritis, there's a lot of information out there—and not all of it is accurate. Misconceptions can keep you from finding effective ways to manage your joint pain and live a full, active life. Let's clear up a few common myths so you can focus on what truly helps your joints feel and move better. Understanding the reality of osteoarthritis is the first step toward taking control of your health.
Myth: It's Just "Wear and Tear"
This is probably the most common thing people hear about osteoarthritis, but it’s a major oversimplification. Calling it simple "wear and tear" suggests that your joints just wear out like old tires, which isn't the whole story. Osteoarthritis is a complex condition where the protective cartilage in your joints breaks down due to a combination of factors. Things like your family history, previous joint injuries, obesity, and repetitive stress all play a significant role. Thinking of it as just wear and tear can make you feel helpless, but knowing the true risk factors gives you areas you can actually work on to protect your joints.
Myth: It Only Affects Older Adults
While it's true that the risk of osteoarthritis increases with age, this condition is not exclusive to seniors. Younger adults can and do develop osteoarthritis, often as a result of a significant joint injury from sports or an accident. It's also more common in women than in men, especially after age 50. Believing it's an "old person's disease" can lead to missed or delayed diagnoses in younger individuals who might dismiss their joint pain as something else. No matter your age, persistent joint pain is worth looking into so you can get the right support and start feeling better sooner.
Myth: Exercise Makes It Worse
The fear that moving will cause more damage is understandable, but it's one of the most harmful myths about osteoarthritis. In reality, inactivity can make your joints even stiffer and your muscles weaker, which worsens the problem. The key is choosing the right kind of movement. Low-impact activities like swimming, walking, and light strength training can strengthen the muscles that support your joints, improve flexibility, and reduce pain. Staying active is one of the most effective ways to manage your symptoms. There are many treatment options available, and gentle movement is a cornerstone of any effective plan.
How to Manage Osteoarthritis by Understanding Its Causes
When you understand what contributes to osteoarthritis, you can take meaningful steps to manage it. While you can’t turn back the clock on a past injury or change your genetic makeup, you have significant influence over lifestyle factors that impact your joint health. Managing osteoarthritis is less about finding a single "cure" and more about creating a holistic plan that reduces stress on your joints, calms inflammation, and supports your body’s natural healing abilities. By focusing on what you can control—like your weight, activity level, and the therapies you choose—you can protect your joints and live more comfortably.
What You Can and Can't Control
It’s true that osteoarthritis is often linked to the breakdown of cartilage over time. But it’s more than simple wear and tear; it’s a condition that affects the entire joint, including the bone and the tissues that hold everything together. This process is driven by inflammation, which causes pain and further damage. While you can’t control factors like age or a genetic predisposition, you can absolutely influence the things that contribute to inflammation and joint stress. You can control your diet, how you move your body, and your weight. Focusing on these controllable factors is the most empowering way to manage your symptoms and slow the progression of the condition.
Protect Your Joints Through Weight Management
Managing your weight is one of the most effective things you can do for your joints, especially your hips and knees. Every extra pound you carry adds several pounds of pressure to these weight-bearing joints, accelerating cartilage wear. But the impact isn't just mechanical. Research shows that fat tissue itself produces proteins that can cause inflammation throughout your body, including in your joints. By maintaining a healthy weight, you’re not just reducing the physical load on your joints; you’re also turning down the dial on the chronic inflammation that makes osteoarthritis worse. It’s a two-for-one benefit that directly protects your joint health.
Natural Ways to Address the Root Cause
True relief from osteoarthritis comes from addressing the root cause—inflammation—not just masking the pain. While medications can offer temporary relief, they often come with side effects and don’t solve the underlying problem. This is why so many people are looking for natural, drug-free options for pain management. Light therapy is a proven, non-invasive approach that works by reducing inflammation at the cellular level and promoting your body’s own healing processes. Instead of just covering up symptoms, it helps create a healthier environment within the joint. This approach gets to the heart of the issue, offering a sustainable way to find relief and improve your joint function.
Find Drug-Free Relief from Osteoarthritis
Living with osteoarthritis doesn't mean you have to rely on a daily regimen of pills or consider invasive procedures. Many people find significant relief by focusing on drug-free strategies that address the root causes of pain and inflammation. The goal is to manage your symptoms effectively so you can get back to doing what you love. By combining professional therapies with simple, supportive lifestyle habits, you can create a comprehensive plan for long-term joint health.
This approach is all about giving your body the tools it needs to heal and function better. It’s not about a quick fix, but rather a sustainable way to reduce discomfort, improve mobility, and feel more in control of your health. From targeted light therapy that calms inflammation to gentle movements that keep your joints fluid, you have powerful options for feeling better without the side effects of medication. Let's explore a few of the most effective drug-free paths to relief.
How Light Therapy Reduces Inflammation and Promotes Healing
If you're looking for a non-invasive, drug-free way to manage osteoarthritis pain, light therapy is an excellent solution. Instead of just masking symptoms, this therapy gets to the heart of the problem. It uses specific wavelengths of light to penetrate deep into your tissues, which helps reduce the inflammation that causes so much of your pain and stiffness. By addressing one of the main sources of arthritis discomfort, light therapy helps your body’s natural healing processes kick in.
This treatment is a gentle yet powerful way to get relief without surgery or heavy medications. It’s a cornerstone of modern pain management because it supports your body from the inside out, helping you regain mobility and improve your quality of life.
Taking a Holistic Approach to Joint Health
While light therapy is incredibly effective on its own, it works even better as part of a holistic health plan. Think of it as a key player on your wellness team. Combining light therapy with other supportive treatments can lead to even better results for your joints. For example, many people find that pairing their sessions with physical therapy, chiropractic care, or massage helps improve joint function and flexibility more quickly.
This integrated approach ensures you’re supporting your body from all angles. By creating a well-rounded strategy, you’re not just treating the pain—you’re investing in long-term preventative wellness that keeps your joints healthy and resilient for years to come.
Simple Lifestyle Changes and Movement Therapies
While professional treatments are vital, the small choices you make every day have a huge impact on your joint health. It’s important to remember that while treatments can’t reverse arthritis, they are highly effective for managing the pain and stiffness it causes. You can support these therapies by incorporating simple habits into your routine.
Gentle, low-impact exercises like walking, swimming, or cycling can keep your joints mobile without adding extra strain. Mindful practices like yoga and tai chi are also fantastic for improving balance and flexibility. Pairing these movements with an anti-inflammatory diet rich in fruits, vegetables, and healthy fats gives your body the nourishment it needs to fight inflammation naturally. These lifestyle adjustments empower you to take an active role in your own relief.
Frequently Asked Questions
Will exercise make my osteoarthritis worse? This is a common fear, but the right kind of movement is actually one of the best things you can do for your joints. Inactivity can lead to more stiffness and muscle weakness, which takes away crucial support from your aching joints. The key is to choose low-impact activities like walking, swimming, or cycling that strengthen the muscles around the joint without causing more strain. It’s all about finding a balance that keeps you moving comfortably.
Is osteoarthritis inevitable as I get older? While the risk does increase with age, joint pain is not a guaranteed part of getting older. Age is just one of several factors, alongside genetics, past injuries, and lifestyle habits. Thinking of it as inevitable can feel discouraging, but the truth is you have a lot of influence over your joint health. Making proactive choices about how you move and what you eat can make a significant difference at any age.
Besides a major injury, what else could have caused my joint pain? Osteoarthritis often develops from the cumulative effect of many small things over a long period. It might not be from a single big injury but rather from years of repetitive motions at your job or during a hobby. Factors like carrying extra weight, your genetic predispositions, and even your diet can contribute to the gradual breakdown of cartilage. It’s rarely one single cause, but a combination of factors unique to your life.
How does managing my weight help with more than just reducing pressure on my joints? Reducing the physical load on your knees and hips is a huge benefit, but it’s only half the story. Fat tissue is metabolically active and produces proteins that can increase inflammation throughout your entire body. This means that maintaining a healthy weight doesn't just ease the mechanical stress on your joints; it also helps lower the overall level of inflammation that contributes to pain and cartilage damage.
How is light therapy different from just taking pain medication? Pain medication can be effective for temporary relief, but it primarily works by masking the symptoms of pain and inflammation. Light therapy takes a different approach by addressing the issue at a cellular level. It uses specific light wavelengths to help reduce underlying inflammation and support your body's natural healing mechanisms. Instead of just turning off the pain signal, it helps create a healthier environment within the joint for more sustainable relief.
Frequently Asked Questions
Is light therapy safe for athletes?

Yes, light therapy is completely safe and highly beneficial for athletes. It promotes faster muscle recovery, reduces inflammation, and supports performance without the risks of medication or downtime. That’s why professional and amateur athletes worldwide rely on it to train smarter and recover quicker.
How many sessions will I need?

The number of sessions varies depending on the type and severity of your condition. Many patients notice improvement after 3–5 sessions, while chronic conditions may require ongoing care for best results. During your initial consultation, we’ll design a personalized treatment schedule tailored to your body’s response and recovery goals.




