
Psoriatic Arthritis Treatment Comparison: Find Your Fit
The conversation around managing psoriatic arthritis often centers on powerful medications that work to calm an overactive immune system. While these treatments can be life-changing, they aren't the only part of the story. Many people are also looking for ways to support their bodies naturally, without adding more drugs to their routine. This comprehensive psoriatic arthritis treatment comparison will cover the full spectrum of care. We’ll look at the roles of conventional DMARDs, biologics, and JAK inhibitors, and also explore how non-invasive therapies can complement your medical plan to help manage pain and inflammation effectively and safely.
Key Takeaways
- Your best treatment plan is unique to you: Finding relief from psoriatic arthritis involves matching the right therapy—whether it's a conventional medication, a biologic, or a non-invasive option—to your specific symptoms, health, and lifestyle.
- Modern medicine and natural therapies can work together: You don't have to choose between conventional treatments and holistic care. Combining your prescribed medication with supportive options like light therapy can lead to more comprehensive symptom management.
- An informed decision is a confident one: Understanding the effectiveness, potential side effects, and monitoring requirements of each treatment is key. Have an open conversation with your doctor to weigh the pros and cons and choose a path you feel good about.
What Is Psoriatic Arthritis?
If you’re dealing with the scaly, itchy patches of psoriasis and have also started noticing joint pain, you might be looking at psoriatic arthritis (PsA). It’s a chronic inflammatory condition where the body’s immune system, which is supposed to protect you, gets confused and starts attacking healthy skin and joint tissues. This mix-up can lead to a wide range of symptoms, from stiff, painful joints to the kind of deep fatigue that makes it hard to get through the day. It’s more than just a skin issue and more than just arthritis—it’s a combination of both.
Unlike some other forms of arthritis, PsA can show up in many different ways. It might affect the small joints in your fingers and toes, your spine, or even the spots where tendons and ligaments attach to your bones. Because it’s a systemic disease, its impact isn’t just skin-deep; the inflammation can affect your entire body. Understanding the nature of this condition is the first step toward effective pain management and finding a treatment plan that helps you feel like yourself again. The goal isn’t just to quiet the symptoms, but to protect your joints from long-term damage and improve your overall quality of life.
The Skin-Joint Connection
For most people, the skin condition psoriasis comes first, sometimes years before any joint issues appear. Psoriatic arthritis is essentially the next chapter of that story, where the inflammation moves beyond the skin and into the joints. This connection is critical because it highlights that PsA is more than just arthritis. It’s a complex condition that can increase the risk of other health problems, including heart disease. Over time, uncontrolled inflammation can lead to permanent joint damage and a lower quality of life, which is why finding the right treatment early on is so important.
Key Symptoms to Watch For
Psoriatic arthritis can be a bit of a chameleon, with symptoms that vary from person to person. One of the most telling signs is dactylitis, where an entire finger or toe swells up, earning it the nickname "sausage digit." Another key symptom is enthesitis, which is pain and tenderness where tendons or ligaments attach to bone, commonly felt in the heel or the sole of the foot. Beyond that, you might experience pain and stiffness in your joints (especially in the morning), nail changes like pitting or separation from the nail bed, and persistent fatigue that doesn’t go away with rest.
PsA vs. Other Types of Arthritis
While all types of arthritis involve joint pain, PsA has a few unique features that set it apart from rheumatoid arthritis (RA) or osteoarthritis (OA). The most obvious difference is the presence of psoriasis. While RA is typically symmetrical (affecting the same joints on both sides of the body), PsA can be asymmetrical. The presence of dactylitis and enthesitis are also strong indicators of PsA. Because the underlying cause is different, treatment often starts with specific medications called disease-modifying antirheumatic drugs (DMARDs) designed to slow the disease’s progression and support your long-term preventative wellness.
What Are Your Treatment Options for Psoriatic Arthritis?
Finding the right approach to manage psoriatic arthritis (PsA) is a personal process, and it often involves a combination of strategies. Your doctor will help you create a plan based on your specific symptoms, their severity, and your overall health. Generally, treatments fall into a few main categories, from conventional medications to supportive, non-invasive therapies. Understanding what’s available is the first step toward feeling more in control and finding what helps you feel and move better. Let's walk through the primary options you'll likely discuss with your healthcare team.
Conventional DMARDs
Disease-modifying antirheumatic drugs, or DMARDs, are often the first line of defense against PsA. These medications work broadly to suppress your body's overactive immune system, which helps reduce inflammation and can prevent long-term joint damage. The most common starting point is Methotrexate (MTX), a medication that has been used for decades. Studies show MTX can effectively improve joint pain, skin issues, and nail problems for many people. While it can be a game-changer, it requires regular monitoring to keep an eye on potential side effects. Your doctor might also consider other DMARDs depending on your specific needs.
Biologic Therapies
If conventional DMARDs aren't providing enough relief, your doctor might suggest a biologic. Unlike DMARDs that have a widespread effect on the immune system, biologics are more targeted. They are genetically engineered proteins that pinpoint specific parts of the immune response that trigger inflammation in PsA. There are several types, including anti-TNF drugs, which are highly effective at improving arthritis, skin and nail symptoms, and preventing further joint damage. These medications are typically given as an injection or infusion, and they represent a significant step forward in managing moderate to severe PsA.
JAK Inhibitors
A newer class of medication, Janus kinase (JAK) inhibitors, offers another targeted approach to treatment. What sets them apart is that they come in pill form, which can be a welcome alternative for those who prefer not to do injections. JAK inhibitors work from inside your cells to disrupt the signaling pathways that cause inflammation. They are a convenient option that doesn't require refrigeration and can be just as effective as some biologics for managing the joint and skin symptoms of psoriatic arthritis. As with any medication, your doctor will discuss the potential benefits and risks to see if it's a good fit for you.
Natural and Non-Invasive Approaches
Many people find that combining medical treatments with natural and non-invasive therapies provides the most comprehensive relief. While lifestyle changes like exercise and a balanced diet are foundational, other approaches can directly address symptoms. These options are excellent for supporting your body without adding more medication to your routine. Light-based therapies, for example, offer a drug-free way to manage chronic pain and inflammation. These treatments work with your body’s natural healing processes to reduce discomfort and improve mobility, making them a safe and effective part of a holistic preventative wellness plan.
How Do Conventional DMARDs Compare?
When you’re first diagnosed with psoriatic arthritis, your doctor will likely talk to you about conventional DMARDs, which stands for Disease-Modifying Antirheumatic Drugs. Think of these as the foundational, first-line-of-defense medications that have been used for years. Their main job is to slow down the disease and prevent further joint damage by calming your overactive immune system.
These medications aren't a quick fix; they can take several weeks or even months to start working. They are often the starting point because they have a long track record and are generally considered safe for long-term use. While newer treatments have since become available, conventional DMARDs remain a crucial part of the PsA treatment puzzle for many people. Understanding how they work and what to expect can help you have a more informed conversation with your doctor about your care plan.
Methotrexate: Efficacy and Safety
If you’ve started researching PsA treatments, you’ve probably come across methotrexate. It’s one of the most common DMARDs prescribed and is often the first one doctors recommend. Studies show it can help with a wide range of PsA symptoms, including joint pain, skin plaques, and even nail issues. While it doesn't work for everyone, a significant number of people find relief with it.
One of the main reasons it’s so widely used is its established safety profile. It’s been around for a long time, so doctors are very familiar with how to monitor it and manage potential side effects. For many, it provides a reliable and low-risk starting point for getting their symptoms under control and improving their overall preventative wellness.
Exploring Other DMARDs
Beyond methotrexate, there are a few other conventional DMARDs your doctor might consider, like sulfasalazine and leflunomide. These medications also work to suppress the immune system but are generally considered to have less robust evidence supporting their use specifically for psoriatic arthritis compared to methotrexate or newer biologic drugs.
That doesn't mean they're not an option, though. Every person's experience with PsA is unique, and what works for one person might not work for another. These other DMARDs can be a good alternative if you can't take methotrexate or if it doesn't provide enough relief on its own. They offer more choices in the toolkit for finding a treatment that fits your specific needs.
When Are Conventional Treatments the Right Choice?
Deciding on a treatment plan is a very personal process. Your doctor will recommend a path forward based on your specific symptoms—whether your PsA primarily affects your joints, skin, spine, or all of the above. The goal is to match the treatment to the type and severity of your disease.
It’s also important to know that finding the right fit can take time. Research shows that about 30-40% of people don’t respond to their first treatment. Unfortunately, there’s no test to predict which medication will work best for you, so it can sometimes feel like trial and error. This is a normal part of the journey, and it’s why having a comprehensive approach to pain management is so important.
What Makes Biologic Treatments Different?
If conventional treatments haven’t given you the relief you need, your doctor might talk to you about biologics. These aren't your typical pills; they are complex drugs derived from living cells. What sets them apart is their precision. Instead of taking a broad approach to suppressing your immune system, biologics are designed to find and block specific proteins that trigger the inflammation behind psoriatic arthritis. Think of it as sending in a special agent to disarm a specific threat, rather than shutting down the whole system.
This targeted action is why biologics can be so effective at managing symptoms and, importantly, slowing down joint damage. Because they work on very specific parts of the immune response, they can offer a different risk-and-reward profile compared to older medications. They are typically given as an injection you can do at home or as an infusion at a clinic. There are several types of biologics, each targeting a different inflammatory pathway, which gives you and your doctor more options to find the one that works best for your body.
Anti-TNF Agents for Joint and Skin Relief
One of the first and most common types of biologics your doctor might discuss are anti-TNF agents. TNF, or tumor necrosis factor, is a protein that signals your body to create inflammation. In autoimmune conditions like PsA, your body makes way too much of it. Anti-TNF drugs work by finding and blocking this protein, which helps calm down the inflammation in your joints and skin.
These medications have a long track record and have been shown to effectively reduce joint swelling, stiffness, and skin plaques. Research shows that about 60% of people who use them experience at least a 20% improvement in their symptoms. They are also proven to help prevent further joint damage, which is a key goal in managing PsA long-term.
IL-17 Inhibitors for Comprehensive Care
Another group of biologics targets a different inflammatory protein called Interleukin-17 (IL-17). These are known as IL-17 inhibitors. They are a great option for many people, whether you’re trying a biologic for the first time or if anti-TNF drugs didn't work well for you. These medications are particularly good at clearing up the skin symptoms of psoriasis, with studies showing many people achieve clear or almost clear skin.
Beyond the skin benefits, IL-17 inhibitors are also very effective for joint pain and can tackle some of the trickier PsA symptoms like enthesitis (inflammation where tendons attach to bone) and dactylitis (swelling of an entire finger or toe). This makes them a strong all-around choice for managing the different ways PsA can affect your body.
The Unique Benefits of IL-12/23 Inhibitors
A third class of biologics targets two other related proteins: Interleukin-12 and Interleukin-23. These drugs, known as IL-12/23 inhibitors, block the signals that lead to inflammation and skin cell overgrowth. They are effective at treating the full range of PsA symptoms, including arthritis, skin plaques, dactylitis, and enthesitis, while also helping to prevent long-term joint damage.
What makes them stand out is their impressive performance in treating enthesitis. One study found that an IL-12/23 inhibitor was more than twice as effective at clearing up enthesitis compared to anti-TNF drugs. For people whose PsA pain is concentrated where tendons and ligaments meet bone, this specific benefit can make a huge difference in their daily comfort and mobility.
How Do JAK Inhibitors Measure Up?
If you're exploring treatment options beyond conventional DMARDs and biologics, you’ll likely come across Janus kinase (JAK) inhibitors. This class of medication represents a different approach to managing psoriatic arthritis. Instead of working outside the cells like biologics, JAK inhibitors work from the inside, interrupting the cellular signals that trigger inflammation.
This unique mechanism offers another path to relief, but it’s important to understand how these treatments stack up in terms of convenience, effectiveness, and safety. For many, they offer a compelling alternative to injections, but they also come with their own set of considerations. Thinking through these points can help you have a more productive conversation with your doctor about whether JAK inhibitors might be a good fit for your treatment plan and lifestyle.
Oral Medication vs. Injections
One of the most significant advantages of JAK inhibitors is that they are taken as a pill, not an injection. If you’re not a fan of needles, this is a major plus. This simple difference can make sticking to your treatment plan much easier.
Beyond avoiding injections, oral medications offer practical benefits. They are typically stable at room temperature, so you don’t have to worry about keeping them refrigerated, which simplifies travel and storage. This convenience factor can make a real difference in your day-to-day life, removing some of the logistical hurdles that can come with injectable psoriatic arthritis treatments.
Efficacy Compared to Biologics
When it comes to getting results, JAK inhibitors hold their own against biologics. In fact, some studies suggest that certain JAK inhibitors may offer faster and more significant improvement than some widely used biologics. For people who haven't had success with other treatments, this can be an encouraging option to explore.
Of course, effectiveness is highly individual. What works wonders for one person might not work as well for another. The goal is to find the treatment that best controls your specific symptoms—whether they affect your joints, skin, or both. Discussing the clinical trial results for different medications with your doctor can help you set realistic expectations.
Key Safety Considerations
With any systemic therapy, it’s crucial to talk about safety. Because JAK inhibitors modify the immune system to reduce inflammation, they can also increase your risk of certain infections. Studies have linked some JAK inhibitors to a higher rate of serious infections compared to other treatments.
This is why your doctor will likely run tests to check for underlying infections before you start and will monitor you closely during treatment. It’s all about finding a balance between managing your PsA symptoms effectively and keeping your overall health protected. Openly discussing these risks will help you and your healthcare provider make a confident and informed decision together.
Are There Natural Options for Psoriatic Arthritis?
If you’re living with psoriatic arthritis (PsA), you’ve likely discussed medications with your doctor. But it’s completely understandable to wonder what else is out there. Many people look for natural ways to manage their symptoms, reduce inflammation, and feel more in control of their health. The great news is that several non-invasive approaches can make a real difference, either by complementing your current medical plan or by providing relief on their own.
Natural options for PsA go beyond just diet and supplements. They include targeted therapies that work with your body’s own healing mechanisms to address both joint pain and skin symptoms. These approaches are often focused on reducing the overall inflammatory burden on your body without the systemic side effects that can come with some medications. By integrating these strategies, you can build a more comprehensive and personalized plan for pain management that aligns with your lifestyle and wellness goals. It’s about creating a supportive environment for your body to thrive, giving you more tools to manage flare-ups and maintain your quality of life.
The Benefits of Light and Laser Therapy
One of the most promising non-invasive treatments for psoriatic arthritis is light therapy. Specific wavelengths of light, including those used in advanced laser therapy, have been shown to calm inflammation and improve skin plaques associated with PsA. This works by targeting inflammation at the cellular level, helping to reduce the swelling and pain in your joints while also clearing up skin symptoms. It’s a gentle yet effective way to get relief right where you need it.
Because it’s a localized treatment, it doesn’t come with the systemic side effects that are a concern with many oral or injectable medications. This makes it an excellent option for long-term preventative wellness and for anyone seeking a drug-free way to manage their condition.
How Natural Treatments Complement Medical Care
Thinking about natural treatments doesn’t mean you have to abandon your conventional medical plan. In fact, they often work best together. An integrative approach that combines lifestyle changes with your prescribed therapies can lead to better overall outcomes. For example, pairing your medication with an anti-inflammatory diet, gentle exercise like yoga or swimming, and stress-reduction techniques can help you manage symptoms more effectively.
This combined strategy allows you to address PsA from multiple angles. While your medication works on the underlying disease process, your lifestyle choices can help reduce triggers and support your body’s overall health. This gives you a more active role in your treatment and can significantly improve your day-to-day well-being.
The Safety of Non-Invasive Approaches
When you’re exploring different treatments, safety is always a top priority. While natural options may not have the same volume of clinical research as pharmaceuticals, they generally have a much lower risk of side effects. Things like changing your diet, getting regular exercise, and quitting smoking are recommended by experts because they are safe and beneficial for your overall health, not just your PsA.
Non-invasive therapies like light and laser therapy are also known for their strong safety profile. They offer a way to directly address pain and inflammation without introducing substances into your body that could cause unwanted reactions. This makes them a reassuring choice for anyone who is sensitive to medications or concerned about long-term side effects. Our holistic approach prioritizes these safe, proven methods to help you feel better.
How Do You Choose the Best Treatment?
Finding the right treatment for psoriatic arthritis is a journey, not a one-stop shop. The best approach for you is one that fits your specific symptoms, your overall health, and your personal comfort level. It’s a decision you’ll make in partnership with your healthcare provider, weighing all the factors to create a plan that helps you feel and move better.
Think of it as building a personalized toolkit for managing your health. What works wonders for one person might not be the right fit for another, and that’s completely normal. The key is to understand your options and feel empowered to choose a path that aligns with your goals. To get there, we’ll walk through three key areas to consider: the severity of your condition, your lifestyle and general health, and your own preferences for care.
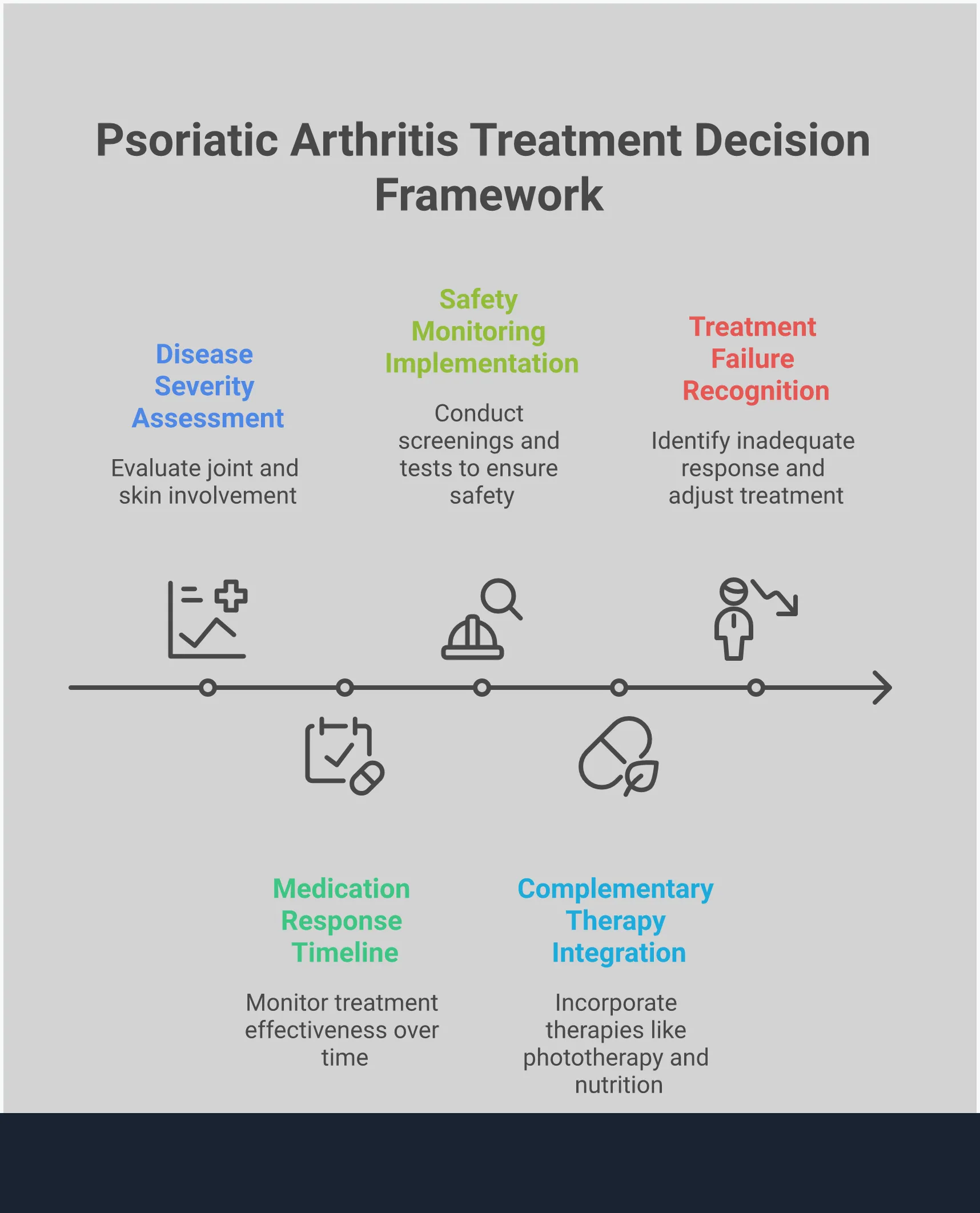
Assess Your Disease Severity
The first step in choosing a treatment is getting a clear picture of how psoriatic arthritis affects your body. Your doctor will look at which areas are most impacted—is it primarily your joints, your skin, or your spine? The severity and location of your symptoms often guide the initial treatment recommendations. For instance, if you’re dealing with severe joint inflammation, your doctor might suggest a biologic therapy like an anti-TNF agent to provide targeted relief.
It’s also helpful to know that finding the right medication can sometimes take a bit of trial and error. Research shows that a significant number of patients don’t get the results they want from their first treatment. This isn’t a setback; it’s a normal part of the process. Being open with your doctor about what is and isn’t working is crucial to finding a treatment that effectively manages your chronic pain.
Consider Your Overall Health and Lifestyle
Your psoriatic arthritis treatment doesn’t exist in a vacuum. It needs to fit into the larger context of your overall health and daily life. Factors like your age, other medical conditions you may have, and your lifestyle all play a role in determining the safest and most effective option. For example, some treatments may be a better choice for older adults because they carry a lower risk of certain side effects.
This is why it’s so important to have an open conversation with your doctor about your complete health history. Be sure to discuss any concerns you have, especially when starting a new medication that might affect your immune system. Your doctor can then create a monitoring plan to ensure your treatment is working as it should without causing other issues. A holistic approach that considers you as a whole person is always the best path forward.
Weigh Your Personal Preferences
Ultimately, you are the most important member of your care team. Your preferences and comfort level matter immensely when choosing a treatment plan. Do you prefer taking a daily pill over receiving an injection? Are you looking for ways to complement your medical treatment with natural, non-invasive options? These are valid and important questions to ask.
Many people find success by integrating natural approaches alongside their conventional medical care. Exploring options like light therapy can be an effective way to manage symptoms and support your body’s healing process without adding more medication. Learning about all the different types of treatments, including their potential risks and benefits, allows you to make an informed decision. Your ideal plan is one that not only works for your body but also feels right for you.
How Do Success Rates and Safety Compare?
When you’re looking at a list of potential treatments, two big questions usually come to mind: "Will it work?" and "Is it safe?" The answers aren't always straightforward, as effectiveness and side effects can vary from person to person. The goal is to find a treatment that not only manages your symptoms but also fits into your life with minimal disruption.
Understanding the potential outcomes and risks is a key part of making an informed decision with your doctor. Let's break down what the research says about success rates, common safety concerns like infection risks, and the long-term monitoring that often comes with conventional psoriatic arthritis treatments. This information can help you weigh the pros and cons as you consider your path forward, whether that involves medication, natural therapies, or a combination of both.
A Look at Remission Statistics
The main goal of any PsA treatment is to reach what doctors call "minimal disease activity," or MDA. This is a state where your symptoms are well-controlled, helping to prevent long-term joint damage and improve your overall quality of life. While modern medications like anti-TNF drugs have shown great success in helping people reach this goal, they don't work for everyone.
Research shows that about 30-40% of patients may not respond well to their first treatment. Since there isn't a test to predict which medication will be the right fit, it can sometimes feel like a process of trial and error. This is why exploring complementary therapies for pain management can be so helpful, offering support while you and your doctor find the best medical approach for you.
Comparing Infection Risks Across Treatments
Because many PsA medications work by suppressing parts of the immune system, one of the most significant safety concerns is an increased risk of infection. While all systemic treatments carry some risk, the level of concern can differ quite a bit between drug classes. It’s a critical factor to discuss with your healthcare provider, especially if you are prone to infections.
For example, studies have linked certain JAK inhibitors to higher rates of serious infections. Some IL-17 inhibitors have also been found to increase the risk of serious side effects after the first few months of use. Understanding these potential risks is essential when weighing your options and deciding what level of risk you are comfortable with for your long-term preventative wellness plan.
Long-Term Monitoring and Side Effects
Taking powerful immune-suppressing medications isn't a "set it and forget it" situation. These treatments require careful and consistent long-term monitoring to catch any potential problems early. Your doctor will likely recommend regular check-ups and screenings, sometimes including annual tests for things like tuberculosis, to ensure the medication is not causing unforeseen issues.
This ongoing supervision is crucial, especially when you first start a new drug. While serious side effects are not common with many modern biologics, the need for vigilance is part of the treatment package. This is another reason many people seek out non-invasive therapies that don't require the same level of medical oversight and can easily be integrated into a holistic health routine.
What Challenges Might You Face?
Finding the right treatment for psoriatic arthritis is a huge step, but the path isn’t always a straight line. It’s completely normal to run into a few bumps along the way. From feeling overwhelmed by choices to figuring out the logistics of care, these hurdles are a real part of the process for many people. Knowing what to expect can help you feel more prepared and in control of your health journey.
The key is to remember that you’re not alone in this. Many people with PsA face similar questions and concerns. The goal is to arm yourself with information, build a strong support system with your healthcare team, and advocate for the care plan that feels right for you. Let’s walk through some of the most common challenges you might encounter and talk about how to approach them with confidence.
Overcoming Decision Fatigue
With so many treatment options available, from pills and injections to light therapy, it’s easy to feel overwhelmed. This "decision fatigue" is a real thing. Doctors often select treatments based on whether your joints, skin, or spine are most affected. However, there’s no single test to predict which medication will work best for you, and it can be discouraging to learn that up to 40% of people may not respond well to their first treatment. The best approach is to have open, ongoing conversations with your doctor. Think of it as a partnership where you work together to find the perfect fit, even if it takes a little time.
Managing Concerns About Side Effects
It’s smart to be mindful of the potential side effects that come with many PsA medications. Every treatment has a different risk profile, and it’s important to weigh the benefits against the potential downsides. For example, some studies show that certain biologic drugs, like IL-17 inhibitors, can increase the risk of serious infections. Understanding these possibilities helps you make a truly informed decision. This is also why many people explore complementary, non-invasive options like light therapy to manage symptoms and support their overall wellness with fewer systemic risks.
Dealing with Insurance and Access Issues
Sometimes, the biggest challenge isn’t medical—it’s logistical. Getting the right treatment can involve navigating insurance approvals, high co-pays, and access hurdles. The reality is that a lack of large-scale studies comparing all the available PsA therapies can make it harder for insurance companies to create clear coverage guidelines. This can be incredibly frustrating when you and your doctor have decided on a plan. Don’t get discouraged. Talk to your doctor’s office about patient assistance programs, and be persistent with your insurance provider. Exploring all your options, including local wellness services with clear membership pricing, can also help you build a comprehensive and accessible care plan.
Common Myths About PsA Treatments
When you’re trying to find the right path forward for managing Psoriatic Arthritis, it’s easy to get tangled up in misinformation. Well-meaning advice from friends, online forums, and outdated articles can create a confusing picture of what treatment really looks like. Let’s clear the air and tackle some of the most common myths head-on. Understanding the truth can help you feel more confident and empowered as you work with your healthcare team to create a plan that truly fits your life and your body’s unique needs.
Myth: There's a One-Size-Fits-All Cure
If only it were that simple! The truth is, Psoriatic Arthritis shows up differently for everyone. One person might struggle primarily with joint pain in their hands, while another deals with spinal inflammation and skin plaques. Because of this, there’s no single treatment that works for everybody. In fact, research shows that up to 40% of patients may not respond well to their first prescribed medication. Your doctor will recommend a treatment based on your specific symptoms, but finding the right fit often involves a bit of trial and error. This is why a personalized approach that includes effective pain management strategies is so important.
Myth: Treatment Effectiveness Is All or Nothing
It’s easy to think of treatment as a simple switch—either it works perfectly, or it doesn’t work at all. In reality, success is often measured in degrees of improvement. The goal is to reach what’s called “minimal disease activity,” a state where your symptoms are low enough to significantly improve your quality of life and prevent long-term joint damage. Even if a treatment doesn’t eliminate every symptom, reducing pain, clearing skin, and improving mobility are major wins. A comprehensive plan focused on preventative wellness can help you achieve these milestones and maintain your progress over time, celebrating every step forward.
Myth: Newer Drugs Are Always the Best Option
We’re often conditioned to believe that the latest innovation is the greatest, but that’s not always the case in medicine. While newer biologic and JAK inhibitor drugs have been game-changers for many, they aren’t automatically superior for every person. Some older, time-tested medications like methotrexate can be highly effective and may even carry a lower risk of certain side effects compared to newer options. The best treatment for you is one that balances effectiveness with a safety profile you’re comfortable with. It’s all about finding what works for your body and aligns with your health philosophy, which is why many people explore safe, non-invasive therapies to complement their medical care.
Frequently Asked Questions
Can I use natural therapies like light therapy along with my prescription medication? Absolutely. In fact, many people find that this kind of combined approach gives them the best results. While your medication works systemically to manage the disease, a non-invasive treatment like light therapy can provide targeted relief for specific areas of pain and inflammation. It's an excellent way to support your body and manage symptoms without adding more drugs and potential side effects to your routine.
Why might I have to try several different medications before finding one that works? This is a very common and normal part of the process, so don't get discouraged. Psoriatic arthritis is a complex condition that affects everyone differently, and right now, there isn't a test that can predict how your body will respond to a specific drug. Think of it as a collaborative journey with your doctor to find the most precise and effective tool for your unique situation.
I don't like needles. Are there effective PsA treatments that aren't injections? Yes, there are several great options if you prefer to avoid injections. The first medications doctors often prescribe, known as conventional DMARDs, are typically pills. Additionally, a newer class of targeted medication called JAK inhibitors also comes in pill form, offering the effectiveness of a biologic without the need for a needle.
What does it really mean for a PsA treatment to be "successful"? Success with psoriatic arthritis treatment isn't about finding a one-time cure, but about achieving long-term control. The goal is to reach what doctors call "minimal disease activity." This means your joint pain and swelling are significantly reduced, your skin is clear or almost clear, and you're able to go about your daily life without major disruption. A successful plan protects your joints from future damage and helps you feel like yourself again.
Are these powerful medications safe to take for many years? This is a very important question. While medications that affect the immune system do come with risks, they have been used for years, and doctors are very experienced in monitoring them safely. Your healthcare team will require regular check-ups to ensure the treatment is working properly without causing other issues. This need for careful oversight is also why many people incorporate safe, non-invasive therapies into their plan to support their overall wellness.
Frequently Asked Questions
Is light therapy safe for athletes?

Yes, light therapy is completely safe and highly beneficial for athletes. It promotes faster muscle recovery, reduces inflammation, and supports performance without the risks of medication or downtime. That’s why professional and amateur athletes worldwide rely on it to train smarter and recover quicker.
How many sessions will I need?

The number of sessions varies depending on the type and severity of your condition. Many patients notice improvement after 3–5 sessions, while chronic conditions may require ongoing care for best results. During your initial consultation, we’ll design a personalized treatment schedule tailored to your body’s response and recovery goals.




